Hesi case study heart failure with atrial fibrillation – Embark on a comprehensive exploration of HESI Case Study: Heart Failure with Atrial Fibrillation, a prevalent cardiac condition affecting millions worldwide. Delve into its complexities, from pathophysiology to management strategies, and witness the transformative power of evidence-based care.
Uncover the intricacies of HESI case studies, a valuable tool for nurses to hone their clinical reasoning skills and deliver exceptional patient care. Through real-world scenarios, we unravel the complexities of heart failure with atrial fibrillation, empowering nurses to make informed decisions and improve patient outcomes.
1. Overview of Heart Failure with Atrial Fibrillation (HFaf): Hesi Case Study Heart Failure With Atrial Fibrillation
Heart failure with atrial fibrillation (HFaf) is a common and debilitating condition characterized by the presence of heart failure symptoms and atrial fibrillation, a type of irregular heart rhythm. HFaf is a major public health concern, affecting millions of people worldwide and significantly impacting their quality of life and mortality.
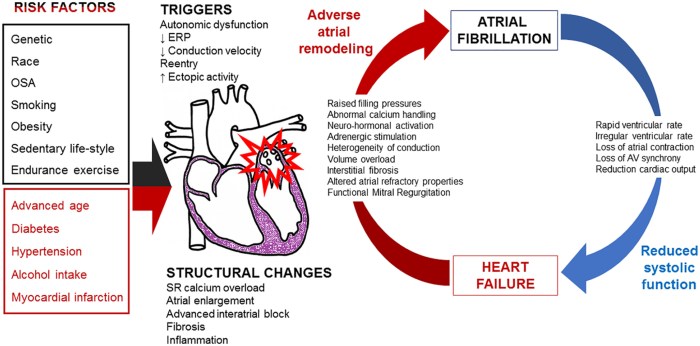
The prevalence of HFaf is estimated to be 1-2% of the general population and increases with age, affecting up to 10% of individuals over the age of 80. The incidence of HFaf is also increasing due to the aging population and the rising prevalence of risk factors such as hypertension, obesity, and diabetes.
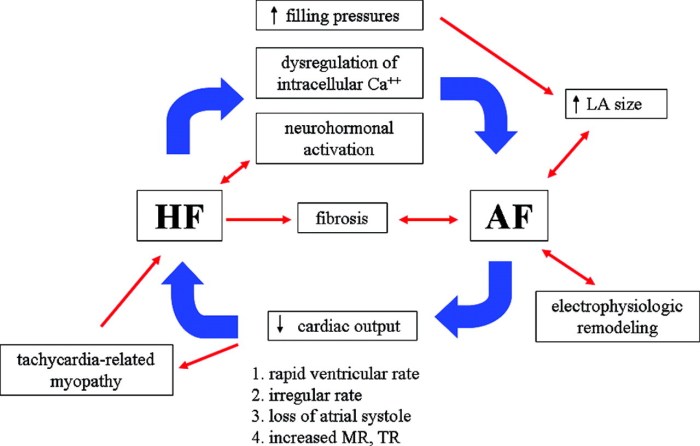
The pathophysiology of HFaf is complex and involves multiple mechanisms. Atrial fibrillation leads to loss of coordinated atrial contraction, which impairs ventricular filling and reduces cardiac output. Additionally, atrial fibrillation promotes the formation of blood clots in the heart, which can lead to embolic events such as stroke.
2. Clinical Presentation and Diagnosis of HFaf
The clinical presentation of HFaf can vary depending on the severity of the condition. Common symptoms include shortness of breath, fatigue, exercise intolerance, and palpitations. Physical examination may reveal signs of heart failure, such as pulmonary edema, jugular venous distension, and peripheral edema.
Electrocardiography (ECG) is essential for diagnosing HFaf and typically shows an irregular atrial rhythm with a rapid ventricular response. Echocardiography is also useful for assessing cardiac structure and function and can help to exclude other causes of heart failure.
The differential diagnosis of HFaf includes other conditions that can cause similar symptoms, such as coronary artery disease, valvular heart disease, and cardiomyopathy. A thorough history and physical examination, along with appropriate diagnostic tests, are necessary to establish the correct diagnosis.
3. Management of HFaf
The goals of treatment for HFaf are to improve symptoms, prevent complications, and prolong survival. Management typically involves a combination of pharmacological therapies, non-pharmacological interventions, and device therapy.
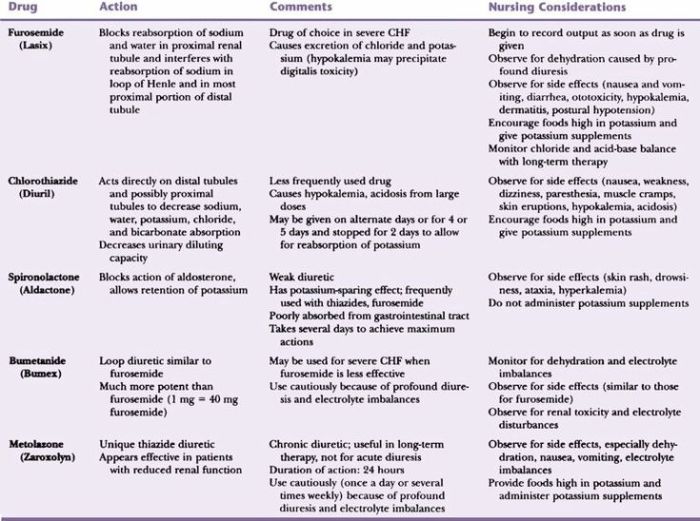
Pharmacological therapies for HFaf include ACE inhibitors, beta-blockers, and diuretics. ACE inhibitors and beta-blockers reduce the workload on the heart and improve cardiac function, while diuretics help to reduce fluid overload.
Non-pharmacological interventions for HFaf include lifestyle modifications, such as weight loss, exercise, and smoking cessation. These measures can help to improve overall health and reduce the risk of complications.
Device therapy may be indicated for patients with HFaf who have severe symptoms or who are at high risk of complications. Pacemakers can be used to control the heart rate and improve cardiac function, while implantable cardioverter-defibrillators (ICDs) can be used to prevent sudden cardiac death.
4. Prognosis and Outcomes of HFaf
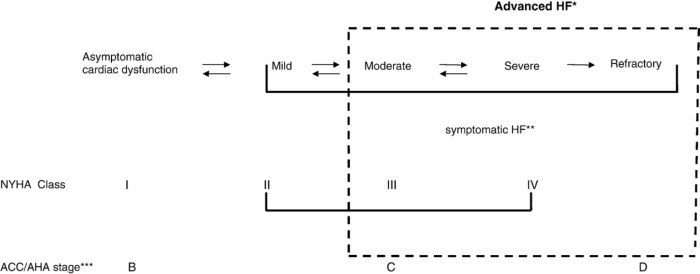
The prognosis of HFaf depends on a number of factors, including the severity of the condition, the presence of comorbidities, and the patient’s age and overall health.
Patients with HFaf have a higher risk of complications, such as stroke, heart failure hospitalization, and death. The typical clinical course of HFaf is characterized by periods of stability and exacerbations, which can lead to a gradual decline in cardiac function and quality of life.
The impact of HFaf on quality of life is significant, with patients experiencing limitations in physical activity, social participation, and emotional well-being. The mortality rate for patients with HFaf is also high, with a 5-year survival rate of approximately 50%.
5. Case Study Analysis
Case Presentation:A 75-year-old male with a history of hypertension and diabetes presents with a 2-week history of progressive shortness of breath and fatigue. He also reports intermittent palpitations and a decreased exercise tolerance.
Physical Examination:Blood pressure 160/90 mmHg, heart rate 120 beats per minute, irregular, respiratory rate 24 breaths per minute, oxygen saturation 92% on room air. Auscultation of the lungs reveals bilateral crackles. Jugular venous distension is present, and there is mild peripheral edema.
Diagnostic Tests:ECG shows atrial fibrillation with a rapid ventricular response. Echocardiography reveals a left ventricular ejection fraction of 45% with mild left ventricular hypertrophy and dilatation. Blood tests show elevated B-type natriuretic peptide (BNP) levels.
Management Plan:The patient was diagnosed with HFaf and started on a treatment regimen that included an ACE inhibitor, a beta-blocker, and a diuretic. He was also advised to make lifestyle modifications, such as losing weight and exercising regularly.
Response to Treatment:The patient’s symptoms improved significantly over the next few weeks. His shortness of breath and fatigue resolved, and his exercise tolerance increased. His ECG showed a slower ventricular response, and his echocardiogram showed an improvement in left ventricular function.
6. Future Directions in HFaf Management
There are a number of emerging therapies and research directions in the management of HFaf. These include new medications, devices, and technologies that have the potential to improve outcomes for patients with this condition.
One promising area of research is the development of novel antiarrhythmic drugs that can effectively control atrial fibrillation and prevent its recurrence. Another area of focus is the development of new heart failure therapies that target specific molecular pathways involved in the pathophysiology of HFaf.
The ongoing research in HFaf management is essential for improving the understanding of this condition and developing new therapies that can improve the quality of life and survival of patients.
FAQ Summary
What is the prevalence of heart failure with atrial fibrillation (HFaf)?
HFaf is a common condition, affecting approximately 1-2% of the population worldwide.
What are the typical symptoms of HFaf?
Symptoms of HFaf include shortness of breath, fatigue, swelling in the legs, ankles, and feet, and irregular heartbeat.
How is HFaf diagnosed?
HFaf is diagnosed based on a combination of symptoms, physical examination findings, and diagnostic tests such as electrocardiography and echocardiography.
What are the treatment options for HFaf?
Treatment options for HFaf include medications, lifestyle modifications, and device therapy. Medications include ACE inhibitors, beta-blockers, and diuretics.
What is the prognosis for patients with HFaf?
The prognosis for patients with HFaf varies depending on the severity of the condition and other factors. With proper management, many patients with HFaf can live long and fulfilling lives.